Lung GGO Insights
DR. CHING-YANG WU
Lung GGO describes a lesion with higher tissue density, appearing as grayish areas on CT scans.
It’s not always lung cancer; it can also result from inflammation, fibrosis, or benign tumors.
Lung cancer is just one possible cause.
Whether surgery is needed depends on a thoracic surgeon’s professional evaluation of the lesion’s size and density.
About DR. CHING-YANG WU
- Thoracic Surgeon, Linkou Chang Gung
- Associate Professor, Chang Gung University
- Associate Professor, Chang Gung Hospital
- Instructor, Thoracic & Cardiovascular Surgery Association
- Instructor, Thoracic Surgery Association

Clinical Experience
SERVICE
Lung Cancer Surgery3D imaging
3D imaging aids tumor resection planning, with CT localization and...

MediastinumHolistic Evaluation
Considers tumor size, location, and involvement of vital organs, followed...

Port Placement SurgeryPort A
Considers the patient's treatment needs and vascular involvement of...

Lung GGOImaging Evaluation
Evaluate size, density changes, and initial imaging...
Key Facts About GGO
Lung GGO can be worrying, but early treatment and regular follow-ups can effectively manage it.
Here are key insights about GGO, explained by Dr. Wu:
Key Factors for GGO Surgery
Whether lung GGO requires surgery depends on its size and density.
Medical consensus recommends active treatment for GGOs larger than 0.7–0.8 cm.
For GGOs between 0.5–0.7 cm, density(consolidation-tumor ratio) becomes the deciding factor.
CT imaging evaluates density, with a lesion considered high-density if the ratio of its solid component diameter to total diameter exceeds 50%.
Patients with a family history of lung cancer or a smoking history are also advised to confirm the diagnosis through biopsy.
Non-Surgical GGO Management
If surgery is not immediately required, the thoracic surgeon will recommend regular CT imaging to monitor changes in the GGO:
a. <0.5 cm: Follow-up every 6–12 months
b. 0.5–0.7 cm, density <50%: Follow-up every 3–6 months
c. 0.5–0.7 cm, density >50%: Follow-up every 3 months
If the GGO remains stable for two years, annual follow-ups may be sufficient.
Consistent imaging settings (e.g., slice thickness) are advised for accurate comparisons.
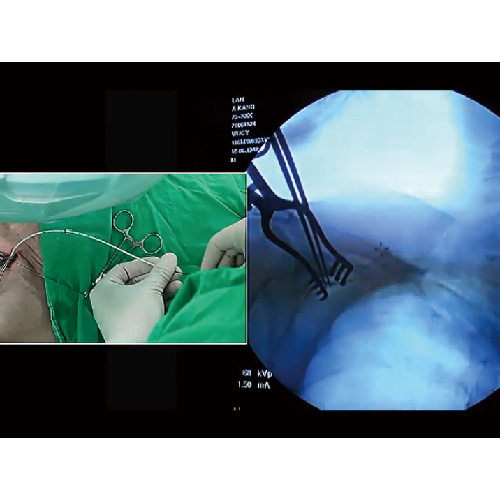
GGO Diagnosis: CT-Guided Biopsy
There are 3 methods to diagnose lung GGO, depending on its location and density.
CT-guided biopsy uses real-time imaging to target and sample the lesion.
For small lesions or those deep in the lung, near fissures, or close to major blood vessels, results may be inconclusive, requiring alternative diagnostic methods.
Possible complications include pneumothorax, hemothorax, or air embolism if the lesion is near blood vessels.
Preoperative imaging can help minimize these risks.
GGO Diagnosis: Bronchoscopic Biopsy
Bronchoscopic biopsy uses a bronchoscope or ultrasound guidance to sample GGO tissue.
This method is limited to lesions within or near the bronchial tree or adjacent lymph nodes.
GGO Diagnosis: Surgical Biopsy
Surgical biopsy is performed when a GGO is highly suspected to be malignant, with no other suspicious lesions and the patient is fit for curative resection.
This approach allows for a definitive diagnosis while enabling immediate treatment if malignancy is confirmed through intraoperative frozen biopsy, reducing the need for multiple procedures.
High-Risk Malignant GGO
Thoracic surgeons first perform a thoracoscopic biopsy of the GGO.
If intraoperative frozen biopsy confirms malignancy, curative resection is conducted through a single-port thoracoscopy, based on preoperative imaging and the patient’s heart and lung function.
GGO Surgery Process
-
 1
1GGO Imaging Diagnosis
Use CT-guided biopsy to assess GGO size and severity.
-
 2
2GGO Surgery Planning
Plan surgery based on GGO size and location.
-
 3
3GGO Surgery Execution
Remove GGO with minimal functional impact.
-
 4
4GGO Margin Assessment
Check for air leaks and place a chest drain.
-
 5
5GGO Follow-Up Plan
Create a follow-up plan with imaging comparisons.

Lung GGO Q&A
Top Questions About Lung GGO, Answered!
What if a Lung GGO is Diagnosed as Malignant?
If a GGO is confirmed malignant through CT or bronchoscopic biopsy, a thoracic surgeon will arrange PET scans and brain MRIs.
These tests assess the severity, including tumor size, lymph node involvement, and possible metastasis, to determine if curative surgery is viable.
What is the Surgical Process for Malignant GGO?
If a GGO is suitable for curative resection, preoperative evaluations assess heart and lung function to determine the resectable lung volume without impairing function.
The surgery is planned to minimize harm, with preoperative CT simulations and tumor localization ensuring safety.
For malignant GGOs, mediastinal lymph node dissection is performed during surgery.
Is Follow-Up Needed After GGO Surgery?
Yes, follow-up is typically required to monitor recovery.
The exact plan depends on the final pathology results.
Discuss with your doctor to ensure optimal post-surgery care.
Lung Tumor Surgery Risks and Alternatives?
Surgery is the best option for malignant tumors if heart and lung function allow for complete resection.
If the biopsy is inconclusive or the tumor is benign, further biopsy or regular imaging follow-up for 2–3 years may be considered.
Get GGOTreatment Now
Specialized Excellence
Trusted Thoracic Care
Dedicated specialists and a trusted team for superior care.

Personalized Surgical Plans
Tailored strategies to minimize functional loss.
Advanced Surgical Skills
Mastery in single-port and robotic thoracic procedures.
Extensive Clinical Expertise
Skilled in treating lung and mediastinal conditions.
Patient-Centered Safety
Tailored care to minimize risks and surgical impact.
Postoperative Monitoring
Ongoing care to ensure no recurrence.
PressCoverage
 Health LTN
Health LTN
Advancing Large-Cell Lung Cancer Treatment: NCYU & Chang Gung Memorial Hospital, Linkou Collaborate
Associate Professor of NCYU and Dr. Wu’s team collaborate on large-cell lung cancer research, yielding significant findings...

Dr. Wu Receives AATS Graham Award at ASCVTS 2016
Dr. Wu excelled in the AATS Graham Award evaluation, delivering his research within the 12-minute limit (10-minute presentation + 2-minute Q&A)...

Dr. Wu’s Team Publishes Study on Three CT-Guided Techniques for Lung Lesion Localization in the European Journal of Radiology!
From September 2019 to August 2021, the team analyzed 418 patients with lung lesions, comparing three CT-guided...

Dr. Wu’s Team Publishes Study on 3D Simulation Training for Oncology Nurses in Seminars in Oncology Nursing!
Since implantable venous catheters are not visible to the naked eye and can only be identified by touch, improper handling may occur...

Dr. Wu’s Research on Implantable Venous Ports Published in Medicine!
Based on literature and clinical experience, Dr. Wu formulated a standard algorithm to evaluate the best entry vessel for...

Dr. Wu’s Lung Cancer Research Published in Medicine!
Many patients still experience recurrent non-small cell lung cancer (NSCLC). To investigate, Dr. Wu and his team reviewed data from 356 stage I lung cancer patients (2005–2011), finding...

Dr. Wu’s Team Publishes Prognostic Study on Lung Adenocarcinomas ≤2cm in the Journal of the Formosan Medical Association!
The study aims to identify unique prognostic factors with clinical significance. Retrospective analysis of cases from...

Dr. Wu’s Team Publishes Study on Postoperative Circulating Tumor Cells as a Predictor of Lung Cancer Recurrence in Diagnostics!
With extensive experience in lung cancer surgery, Dr. Wu’s team investigated whether changes in circulating tumor cells (CTC)...

Dr. Wu’s Study on Central Venous Catheter Tip Placement Published in Medicine!
After analyzing 346 cases, Dr. Wu found that 221 cases (63.9%) were in the non-migration group, 67 cases (19.4%)...

Dr. Wu’s Research on a New Implantable Injection Port Published in Journal of Biomedical Materials Research Part B: Applied Biomaterials!
With in-depth studies and extensive clinical experience in implantable intravenous ports, Dr. Wu has explored complications...

Dr. Wu’s Expertise
- 2011 Taiwan Thoracic & Cardiovascular Surgery New Scholar Award
- 2012 Taiwan Thoracic & Cardiovascular Surgery President’s Award
- 2014 Taiwan Vascular Surgery Smart Award
- 2015 Taiwan Vascular Surgery Smart Award
- 2016 AATS Graham Award
- 2020 Taiwan Thoracic & Critical Care Medicine Best Paper
- 2021 Taiwan Thoracic & Cardiovascular Surgery President’s Award
- 2023 Global Injection Port Consensus Conference
InfoVideo
What Is a Port-A?
Port-A types can be classified by catheter material, high-pressure compatibility, and injection port material. Catheters are mainly made of silicone…
Why Get a Port-A?
A brief overview of the reasons for Port-A placement…

What Is a High-Pressure Port-A?
An overview of high-pressure Port-A and its clinical benefits…

How Do Healthcare Providers Use a High-Pressure Port-A?
Identification and injection procedure for high-pressure Port-A…

Post-Op Care for Port-A
Daily activities remain unrestricted, but certain movements depend on port placement…

Port-A Placement: What to Expect
An implantable venous port, commonly known as a Port-A, serves as a reliable IV access for clinical treatments. It functions like an invisible socket placed under the skin, allowing injection needles—like…