Lung Cancer Surgery Basics
- Tumor malignancy is confirmed through biopsy and pathology analysis.
- Operability depends on clinical staging from preoperative imaging.
- Post-surgery systemic treatment is determined by pathological staging.
- Follow-up with CT imaging varies based on pathological staging.
Criteria for Lung Cancer Surgery
To answer this, it’s important to understand the types of lung lesions and which require further tissue diagnosis and a surgical plan.
GGO, Lung Nodules, and Lung Tumors
These terms describe imaging characteristics of lung lesions on CT scans:
‧GGO: Lesions denser than normal lung tissue, appearing hazy like frosted glass on imaging.
‧Lung Nodules: Lesions smaller than 3 cm.
‧Lung Tumors: Lesions larger than 3 cm.
These terms do not confirm malignancy. A tissue biopsy and pathological analysis are required to determine if a lesion is cancerous.
Malignancy Risk
Based on data from Mount Sinai Medical Center, the risk of malignancy within a year increases with lesion size:
‧>0.5 cm: 3.5% risk within one year
‧>0.6 cm: 5.5% risk within one year
‧>0.7 cm: 7.5% risk within one year
‧>0.8 cm: 10.4% risk within one year
‧>0.9 cm: 13.2% risk within one year
Lesions over 0.7–0.8 cm carry a higher malignancy risk and should be evaluated further.
Lymph Node Metastasis Risk
The risk of lymph node metastasis increases with tumor size, impacting prognosis:
‧<1 cm: 3.8% risk
‧1–2 cm: 16.7% risk
‧2–3 cm: 19.6% risk
‧>3 cm: 37% risk
Tumors smaller than 1 cm, even if malignant, carry a lower risk of lymph node involvement.
Timing for Tissue Biopsy
Studies show that lesion size is closely linked to malignancy risk.
It is medically recommended to perform a tissue biopsy for definitive diagnosis when the lesion reaches 0.7–0.8 cm or larger.
Tumor Staging Assessment
‧Use imaging to determine if the lesion is suitable for curative resection.
‧Evaluate heart and lung function to ensure sufficient lung volume remains for normal breathing post-surgery.
Pre-Surgery Instructions
‧Practice lung recovery exercises using a spirometer.
‧Avoid food and water after midnight the day before surgery.
Surgical Planning
‧Create 3D imaging of lung lesions pre-surgery.
‧Use CT-guided localization for target lesions.
Post-Surgery Care
‧Care for surgical wounds.
‧Use pain medication to manage discomfort and support thoracic rehab.
‧Practice lung recovery with a spirometer.
‧Train to cough effectively to clear airway secretions.
‧Monitor chest tube drainage for air leaks, subcutaneous emphysema, or chylothorax.
‧Encourage mobility to prevent postural hypotension.
DR. CHING-YANG WU
Precise Tumor Resection, Lung Function Preservation
Focused on removing tumors while preserving healthy lung tissue.

Preoperative Assessment
nsures no tumor spread and confirms surgical readiness.
Surgical Simulation
3D imaging and simulation improve surgical planning and precision.
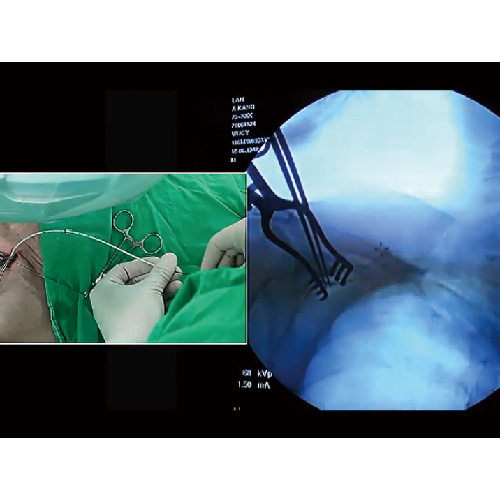
High-Resolution Endoscopy and Single-Port Surgery
Minimizes trauma with accurate, high-resolution techniques.
Faster Recovery
Minimally invasive single-port surgery reduces pain and shortens hospital stays.
Research Excellence
Recognized with top awards(AATS Graham Award) for lung cancer research.
Thoracic Surgeon
DR. CHING-YANG WU
Lung surgery is complex, demanding advanced techniques and a skilled thoracic surgeon for the best results.
Single-Port Lung Tumor Surgery|Single-Port Robotic Lung Surgery|Single-Port Mediastinal Surgery|Injection Port Placement|Ground-Glass Opacity Management
About DR. CHING-YANG WU
- Thoracic Surgeon, Linkou Chang Gung
- Associate Professor, Chang Gung University
- Associate Professor, Chang Gung Hospital
- Instructor, Thoracic & Cardiovascular Surgery Association
- Instructor, Thoracic Surgery Association

Lung Cancer Surgery Steps
-
 1
1Tumor Marking
Mark the lung tumor location using imported CT images.
-
 2
2Resection Simulation
Map lung segment, vessels, and bronchial pathways.
-
 3
3Assess Tumor Volume
Assess resection volume and vessel ligation.
-
 4
4Tumor Localization
Use CT-guided dye for positioning.
-
 5
5Surgical Resection
Precisely resect with CT guidance.

Thoracic Booking
Chang GungTaoyuan
- Address:No. 123, Dinghu Rd., Guishan Dist., Taoyuan City
- Call to Book:03-3196200
- Clinic Hours:Thu. 8:30 AM – 12:00 PM
- Book Now:Taoyuan Chang Gung Thoracic Surgery
Chang GungLinkou
- Address:No. 5, Fuxing St., Guishan Dist., Taoyuan City
- Call to Book:03-3281200
- Clinic Hours:Fri. 1:00 PM – 5:00 PM
- Book Now:Linkou Chang Gung Thoracic Surgery
Lung Cancer Surgery
AWARDS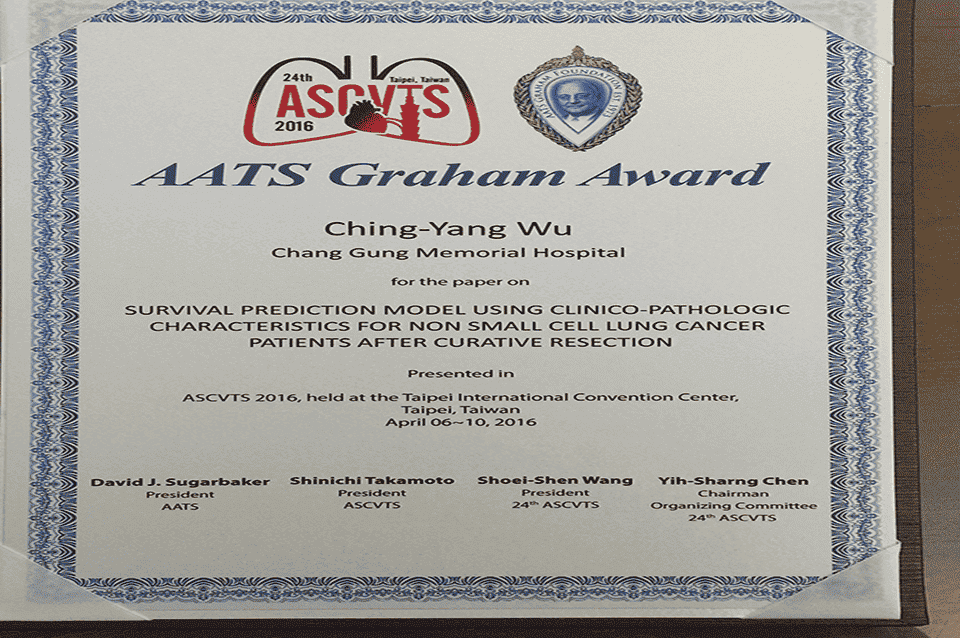
Taiwan Society for Vascular SurgeryTSVSAward

AATSRecognitionGraham Award
Analyzing tumor stages guides personalized follow-up plans for...
TSPCCM2020Best Paper of the Year
Tracking tumor cells pre- and post-surgery identifies high...
TATCS2021President’s Award
Analyzing tumor size, density, and microscopic features on CT scans...

Lung Cancer Resection Q&A
Lung cancer symptoms require tailored surgeries. Find answers to common questions here:
What are the types of lung cancer surgeries?
‧By incision size: Minimally invasive/Open surgery
‧By technique: Thoracoscopic/Robotic surgery
‧By resection scope: Wedge resection/Segmentectomy/Lobectomy
Hospital Stay for Lung Cancer Surgery?
Around 5–8 days, including 3–5 days for preoperative preparation and 2–3 days for recovery.
Are there any postoperative complications?
Common thoracic surgery complications, which mostly are manageable with medication:
‧Air leaks/Subcutaneous emphysema (chest or neck)/Voice changes
‧Chylothorax
‧Lung collapse
‧Chest wound pain or numbness
‧Persistent cough
Why can’t some lung cancer patients undergo surgery?
There are two main reasons:
‧The tumor has spread to vital chest structures, contralateral mediastinum, supraclavicular lymph nodes, or distant sites (stages 3B or 4), making complete resection impossible.
‧The tumor is resectable, but the patient’s heart and lung function cannot tolerate the loss of lung capacity caused by surgery.
Can lung cancer be surgically removed?
Surgical eligibility depends on tumor severity, assessed through imaging for tumor size, lymph node involvement, and metastasis.
Patients with stage 3A or lower, where the tumor is confined to the same side of the chest without critical structure invasion, may undergo complete resection if heart and lung function allow.
Is Post-Surgery Treatment Needed?
Post-surgery treatment depends on pathological staging:
‧Stage 1A1: Regular follow-ups only.
‧Stage 1A2 or 1A3: Follow-up or optional additional treatment.
Stage 2 or higher: Typically 4–6 cycles of chemotherapy with regular check-ups.
If recurrence risks are found, additional chemotherapy may be advised.
Differences Between Clinical and Pathological Staging
Clinical Staging
‧Uses CT, PET, and MRI. for initial evaluation.
‧Evaluates tumor size, lymph nodes, and metastasis.
‧Based on imaging, suited for non-surgical patients.
‧Limited by imaging, unable to detect microscopic lesions.
Pathological Staging
‧Requires tumor removal and microscopic analysis.
‧Assesses tumor invasion and guides treatments.
‧More precise for planning further care.
Is Lung Cancer Surgery Successful?
Lung cancer surgery success depends on preoperative evaluation and patient factors like heart-lung function.
Most tumors can be fully removed, with less than 1% risk of discovering metastasis requiring a treatment change.
Breathing issues post-surgery are uncommon. Vascular injury during vessel ligation occurs in about 1% of cases, which may require open surgery for repair.
PressCoverage
 Health LTN
Health LTN
Advancing Large-Cell Lung Cancer Treatment: NCYU & Chang Gung Memorial Hospital, Linkou Collaborate
Associate Professor of NCYU and Dr. Wu’s team collaborate on large-cell lung cancer research, yielding significant findings...

Dr. Wu Receives AATS Graham Award at ASCVTS 2016
Dr. Wu excelled in the AATS Graham Award evaluation, delivering his research within the 12-minute limit (10-minute presentation + 2-minute Q&A)...

Dr. Wu’s Team Publishes Study on Three CT-Guided Techniques for Lung Lesion Localization in the European Journal of Radiology!
From September 2019 to August 2021, the team analyzed 418 patients with lung lesions, comparing three CT-guided...

Dr. Wu’s Team Publishes Study on 3D Simulation Training for Oncology Nurses in Seminars in Oncology Nursing!
Since implantable venous catheters are not visible to the naked eye and can only be identified by touch, improper handling may occur...

Dr. Wu’s Research on Implantable Venous Ports Published in Medicine!
Based on literature and clinical experience, Dr. Wu formulated a standard algorithm to evaluate the best entry vessel for...

Dr. Wu’s Lung Cancer Research Published in Medicine!
Many patients still experience recurrent non-small cell lung cancer (NSCLC). To investigate, Dr. Wu and his team reviewed data from 356 stage I lung cancer patients (2005–2011), finding...

Dr. Wu’s Team Publishes Prognostic Study on Lung Adenocarcinomas ≤2cm in the Journal of the Formosan Medical Association!
The study aims to identify unique prognostic factors with clinical significance. Retrospective analysis of cases from...

Dr. Wu’s Team Publishes Study on Postoperative Circulating Tumor Cells as a Predictor of Lung Cancer Recurrence in Diagnostics!
With extensive experience in lung cancer surgery, Dr. Wu’s team investigated whether changes in circulating tumor cells (CTC)...

Dr. Wu’s Study on Central Venous Catheter Tip Placement Published in Medicine!
After analyzing 346 cases, Dr. Wu found that 221 cases (63.9%) were in the non-migration group, 67 cases (19.4%)...

Dr. Wu’s Research on a New Implantable Injection Port Published in Journal of Biomedical Materials Research Part B: Applied Biomaterials!
With in-depth studies and extensive clinical experience in implantable intravenous ports, Dr. Wu has explored complications...

Dr. Wu’s Expertise
- 2011 Taiwan Thoracic & Cardiovascular Surgery New Scholar Award
- 2012 Taiwan Thoracic & Cardiovascular Surgery President’s Award
- 2014 Taiwan Vascular Surgery Smart Award
- 2015 Taiwan Vascular Surgery Smart Award
- 2016 AATS Graham Award
- 2020 Taiwan Thoracic & Critical Care Medicine Best Paper
- 2021 Taiwan Thoracic & Cardiovascular Surgery President’s Award
- 2023 Global Injection Port Consensus Conference
Lung CancerGet Immediate Help
InfoVideo
What Is a Port-A?
Port-A types can be classified by catheter material, high-pressure compatibility, and injection port material. Catheters are mainly made of silicone…
Why Get a Port-A?
A brief overview of the reasons for Port-A placement…

What Is a High-Pressure Port-A?
An overview of high-pressure Port-A and its clinical benefits…

How Do Healthcare Providers Use a High-Pressure Port-A?
Identification and injection procedure for high-pressure Port-A…

Post-Op Care for Port-A
Daily activities remain unrestricted, but certain movements depend on port placement…

Port-A Placement: What to Expect
An implantable venous port, commonly known as a Port-A, serves as a reliable IV access for clinical treatments. It functions like an invisible socket placed under the skin, allowing injection needles—like…