Types of Lung Cancer Cells
Non-Small Cell Lung CancerEpithelial Origin
- Adenocarcinoma
- Squamous Cell Carcinoma
- Large Cell Carcinoma
Small Cell Lung CancerNeuroendocrine Cells
- Small Cell Carcinoma
- Carcinoid Tumor
Lung Cancer Essentials
Lung Cancer Incidence
Lung cancer ranks second in overall cancer incidence in Taiwan, with 72.71 cases per 100,000 people.
When carcinoma in situ is included, the incidence rises to 76.67 cases per 100,000, placing lung cancer third among all cancers.
Lung Cancer Mortality Rate
Lung cancer is the leading cause of cancer-related death in Taiwan, with 42.95 deaths per 100,000 people.
It is the top cause of cancer death for both men and women, with 54.71 deaths per 100,000 among men and 31.41 per 100,000 among women.
Assessing Lung Cancer Staging (Severity)
Medical imaging tools used to determine lung cancer staging include:
‧CT Scan: Evaluates tumor size, number, and local invasion.
‧PET Scan: Detects metastasis outside the brain.
‧Brain MRI: Complements PET by assessing possible brain involvement.
Low-dose lung CT may miss lesions smaller than the imaging slice thickness. PET scans typically require tumors to be larger than 0.5 cm to detect abnormal glucose metabolism.
Lung Cancer Treatment
Lung cancer treatment plans vary depending on the clinical stage of the tumor:
‧Tumor limited to one lung lobe or segment, no lymph node involvement → Surgery is the first choice
‧Tumor confined to the same side of the chest, no invasion or major lymph node enlargement → Surgery may be considered, with further treatment based on pathology results
‧Tumor spread beyond one side of the chest → Start with systemic therapy; surgery may follow if the tumor becomes operable
Postoperative Care
‧Pathologic Stage IA1: Regular follow-ups with scheduled CT scans are sufficient
‧Pathologic Stage IA2 or IA3: Options include routine follow-up or additional systemic therapy
‧Routine imaging follow-up helps detect small lesions missed before surgery, improving long-term outcomes.
Lung Cancer Symptoms
Lung cancer symptoms are often vague and non-specific. In the early stages, most patients show no noticeable signs, as the tumor has not yet affected other organs or significant lung function.
As the tumor progresses, symptoms may result from local invasion or distant metastasis. These are commonly due to compression or infiltration of the trachea, veins, or surrounding tissues, and may include:
‧Wheezing
‧Facial swelling
‧Coughing up blood
‧Fever
‧Back pain
‧Headache
Thoracic Surgeon
DR. CHING-YANG WU
The lung surgery is complex and highly difficult, with different surgical methods for treatment. The success of the surgery highly depends on the experience and skill of the thoracic surgeon.
Single-port thoracoscopic surgery for lung cancer/lung tumors
Single-port robotic surgery for lung cancer/lung tumors
Single-port thoracoscopic surgery for mediastinal tumors
Intravenous port implantation (Chemoport)
Follow-up and treatment of lung ground-glass opacities
About DR. CHING-YANG WU
- Attending Thoracic Surgeon at Linkou Chang Gung Memorial Hospital
- Associate Professor of Surgery at Chang Gung University
- Associate Professor of Surgery at Chang Gung Memorial Hospital
- Instructor of the Taiwan Society of Thoracic and Cardiovascular Surgery
- Instructor of the Taiwan Society of Thoracic Surgery


Thoracic Booking
Chang GungTaoyuan
- Address:No. 123, Dinghu Rd., Guishan Dist., Taoyuan City
- Call to Book:03-3196200
- Clinic Hours:Thu. 8:30 AM – 12:00 PM
- Book Now:Taoyuan Chang Gung Thoracic Surgery
Chang GungLinkou
- Address:No. 5, Fuxing St., Guishan Dist., Taoyuan City
- Call to Book:03-3281200
- Clinic Hours:Fri. 1:00 PM – 5:00 PM
- Book Now:Linkou Chang Gung Thoracic Surgery
Additional Treatment Options for Lung Cancer
- Risk Factors for Recurrence: A higher risk of recurrence is present if the postoperative pathology report shows micropapillary or solid components within adenocarcinoma cells, spread of tumor cells through air spaces (STAS), or invasion into the visceral pleura, lymphatic vessels, or blood vessels.
- Postoperative Follow-Up and Treatment Decisions:
‧Without genetic testing: Patients may proceed directly to 4–6 cycles of chemotherapy.
‧With genetic testing: Targeted therapy is selected based on the test results. If no suitable targeted therapy is found, chemotherapy is still required.- Genetic Mutation Testing: The choice of testing panels depends on the tumor type and may incur additional costs. Based on the results, precision medications may be prescribed. If no actionable mutations are found, patients will still require adjuvant chemotherapy.
- Treatment Recommendation for Stage II and Above: Patients with Stage II or higher are advised to undergo adjuvant systemic therapy, along with regular imaging follow-ups to monitor disease progression.
Lung Cancer Surgery Process
-
 1
1Staging Evaluation
The overall severity of the disease is assessed through imaging tools such as CT scans and PET scans
-
 2
2Pre-op Assessment
Imaging data is used to confirm the tumor location, simulate resection options, and create a personalized surgical plan
-
 3
3Precise Tumor Resection
The tumor is surgically removed with targeted techniques to minimize damage to surrounding lung function
-
 4
4Post-op Care
The resected tumor is sent for pathological analysis to guide further treatment planning
-
 5
5Follow-Up Planning
A comprehensive follow-up plan is developed based on the treatment strategy, with systematic comparisons made using follow-up imaging studies
Expert Care for Lung Tumors Starts Here

Lung Cancer FAQ
Here are some common questions about lung cancer to help you better understand treatment options and surgical risks.
What are the types of lung cancer surgery?
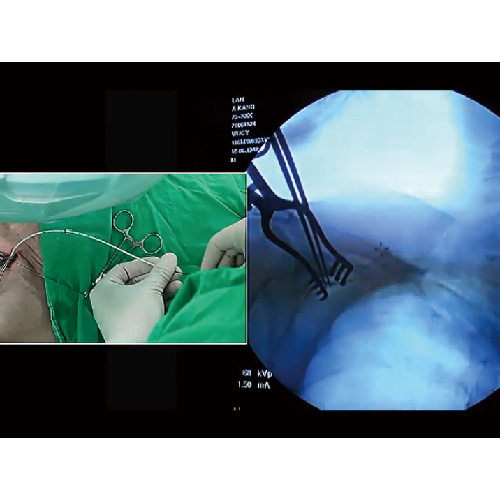
Lung cancer surgeries are classified based on the extent of resection, including wedge resection, segmentectomy, lobectomy (single or bilobectomy), and pneumonectomy. Most procedures today are performed using video-assisted thoracoscopic surgery (VATS) through a single incision. With advancements in surgical technology, robot-assisted single-incision surgery is also now an option for many patients.
How do clinical and pathological staging differ?
Cancer staging is based on the tumor’s size, lymph node involvement, and distant spread. Clinical staging uses imaging and can be limited by resolution—small or low-metabolism tumors may be underestimated.
Pathological staging examines the tumor under a microscope after surgery and provides a more accurate picture of tumor spread.
Think of it like using finer mesh: pathology catches more. About 10% of patients are upstaged after surgery, which can impact further treatment.
How is lung cancer treated?
Treatment strategies depend on the stage of the tumor. If the cancer is limited to a single lung lobe or has only spread to lymph nodes on the same side of the mediastinum, options include surgery alone or surgery combined with neoadjuvant therapy.
If the cancer has spread beyond the same side of the chest, systemic treatment becomes the main approach, which may include targeted therapy, immunotherapy, or chemotherapy.
Is lung tumor surgery risky? Are there alternative treatments?
If the tumor is confirmed to be malignant, and the patient has adequate heart and lung function, complete surgical resection is the standard and most effective treatment according to current guidelines.
If the biopsy does not confirm malignancy—possibly due to limited sample size or a truly benign tumor—repeat biopsy or regular imaging follow-up for 2–3 years may be considered.
PressCoverage
 Health LTN
Health LTN
Advancing Large-Cell Lung Cancer Treatment: NCYU & Chang Gung Memorial Hospital, Linkou Collaborate
Associate Professor of NCYU and Dr. Wu’s team collaborate on large-cell lung cancer research, yielding significant findings...

Dr. Wu Receives AATS Graham Award at ASCVTS 2016
Dr. Wu excelled in the AATS Graham Award evaluation, delivering his research within the 12-minute limit (10-minute presentation + 2-minute Q&A)...

Dr. Wu’s Team Publishes Study on Three CT-Guided Techniques for Lung Lesion Localization in the European Journal of Radiology!
From September 2019 to August 2021, the team analyzed 418 patients with lung lesions, comparing three CT-guided...

Dr. Wu’s Team Publishes Study on 3D Simulation Training for Oncology Nurses in Seminars in Oncology Nursing!
Since implantable venous catheters are not visible to the naked eye and can only be identified by touch, improper handling may occur...

Dr. Wu’s Research on Implantable Venous Ports Published in Medicine!
Based on literature and clinical experience, Dr. Wu formulated a standard algorithm to evaluate the best entry vessel for...

Dr. Wu’s Lung Cancer Research Published in Medicine!
Many patients still experience recurrent non-small cell lung cancer (NSCLC). To investigate, Dr. Wu and his team reviewed data from 356 stage I lung cancer patients (2005–2011), finding...

Dr. Wu’s Team Publishes Prognostic Study on Lung Adenocarcinomas ≤2cm in the Journal of the Formosan Medical Association!
The study aims to identify unique prognostic factors with clinical significance. Retrospective analysis of cases from...

Dr. Wu’s Team Publishes Study on Postoperative Circulating Tumor Cells as a Predictor of Lung Cancer Recurrence in Diagnostics!
With extensive experience in lung cancer surgery, Dr. Wu’s team investigated whether changes in circulating tumor cells (CTC)...

Dr. Wu’s Study on Central Venous Catheter Tip Placement Published in Medicine!
After analyzing 346 cases, Dr. Wu found that 221 cases (63.9%) were in the non-migration group, 67 cases (19.4%)...

Dr. Wu’s Research on a New Implantable Injection Port Published in Journal of Biomedical Materials Research Part B: Applied Biomaterials!
With in-depth studies and extensive clinical experience in implantable intravenous ports, Dr. Wu has explored complications...

Dr. Wu’s Expertise
- 2011 Taiwan Thoracic & Cardiovascular Surgery New Scholar Award
- 2012 Taiwan Thoracic & Cardiovascular Surgery President’s Award
- 2014 Taiwan Vascular Surgery Smart Award
- 2015 Taiwan Vascular Surgery Smart Award
- 2016 AATS Graham Award
- 2020 Taiwan Thoracic & Critical Care Medicine Best Paper
- 2021 Taiwan Thoracic & Cardiovascular Surgery President’s Award
- 2023 Global Injection Port Consensus Conference
InfoVideo
What Is a Port-A?
Port-A types can be classified by catheter material, high-pressure compatibility, and injection port material. Catheters are mainly made of silicone…
Why Get a Port-A?
A brief overview of the reasons for Port-A placement…

What Is a High-Pressure Port-A?
An overview of high-pressure Port-A and its clinical benefits…

How Do Healthcare Providers Use a High-Pressure Port-A?
Identification and injection procedure for high-pressure Port-A…

Post-Op Care for Port-A
Daily activities remain unrestricted, but certain movements depend on port placement…

Port-A Placement: What to Expect
An implantable venous port, commonly known as a Port-A, serves as a reliable IV access for clinical treatments. It functions like an invisible socket placed under the skin, allowing injection needles—like…