What Is the Mediastinum?
The mediastinum is the central compartment of the chest cavity, located between the lungs. It extends from the sternum in the front to the spine in the back, and from the diaphragm at the bottom to the thoracic inlet at the top.
This area contains several vital structures, including the heart (within the pericardium), major blood vessels (such as the aorta, superior vena cava, pulmonary arteries and veins), trachea, esophagus, thymus gland, lymph nodes, and important nerves such as the vagus nerve and phrenic nerve. The mediastinum is commonly divided into four anatomical compartments:
- Superior mediastinum: Located at the top, containing the great vessels, trachea, and esophagus.
- Anterior mediastinum: Situated in front of the heart, primarily composed of connective tissue, fat, and lymph nodes.
- Middle mediastinum: Contains the heart and the pericardium.
- Posterior mediastinum: Located behind the heart, housing the esophagus, descending aorta, and certain nerve structures.
Common Types of Mediastinal Tumors
Thymoma
Thymoma is a common mediastinal tumor, usually benign. Its malignant form is called thymic carcinoma. It’s often linked to autoimmune diseases like myasthenia gravis.

Intrathoracic Thyroid Nodule
In some cases, the thyroid gland may grow downward from the neck into the chest cavity, a condition known as substernal or retrosternal thyroid extension. This often involves the thyroid extending into the superior mediastinum.
Lymphoma
Lymphoma is a tumor that originates in the lymphatic system and can occur in mediastinal lymph nodes. The most common types are Hodgkin lymphoma and non-Hodgkin lymphoma.
Neurogenic Tumor / Schwannoma
These tumors arise from nerve tissue, usually in the posterior mediastinum. Most are benign, but may compress nearby nerves.
Teratoma
Teratoma is a benign tumor composed of various tissue types, such as skin, bone, or hair, and is typically located in the anterior mediastinum, often near the thymus.
Neuroblastoma
Neuroblastoma is a malignant tumor of immature nerve cells, most commonly found in children and typically located in the mediastinum along the sympathetic nervous system, especially near the adrenal glands or in the chest.
Thoracic Surgeon for Mediastinal Tumors
DR. CHING-YANG WU
The lung surgery is complex and highly difficult, with different surgical methods for treatment. The success of the surgery highly depends on the experience and skill of the thoracic surgeon.
Single-port thoracoscopic surgery for lung cancer/lung tumors
Single-port robotic surgery for lung cancer/lung tumors
Single-port thoracoscopic surgery for mediastinal tumors
Intravenous port implantation (Chemoport)
Follow-up and treatment of lung ground-glass opacities
About DR. CHING-YANG WU
- Attending Thoracic Surgeon at Linkou Chang Gung Memorial Hospital
- Associate Professor of Surgery at Chang Gung University
- Associate Professor of Surgery at Chang Gung Memorial Hospital
- Instructor of the Taiwan Society of Thoracic and Cardiovascular Surgery
- Instructor of the Taiwan Society of Thoracic Surgery


Thoracic Booking
Chang GungTaoyuan
- Address:No. 123, Dinghu Rd., Guishan Dist., Taoyuan City
- Call to Book:03-3196200
- Clinic Hours:Thu. 8:30 AM – 12:00 PM
- Book Now:Taoyuan Chang Gung Thoracic Surgery
Chang GungLinkou
- Address:No. 5, Fuxing St., Guishan Dist., Taoyuan City
- Call to Book:03-3281200
- Clinic Hours:Fri. 1:00 PM – 5:00 PM
- Book Now:Linkou Chang Gung Thoracic Surgery
Get Expert Care forMediastinal Tumors
What Causes Mediastinal Tumors?
Mediastinal tumors can arise from a variety of medical conditions, including infections, neoplastic growths (tumors), and inflammatory diseases.
These tumors may originate from different types of tissues and are generally classified as either benign or malignant, depending on the nature of the tumor cells and their behavior.
Causes of Mediastinitis (Mediastinal Inflammation)
Mediastinitis can result from several underlying conditions, including:
- Fungal infections
- Esophageal perforation – A tear or hole in the esophagus that allows bacteria to spread into the mediastinum
- Postoperative infection – Particularly after cardiac or pulmonary surgery
- Spread of nearby infections – Such as infections from adjacent areas, or dental infections that spread downward through muscle fascia into the mediastinum
Clinical Symptoms of Mediastinal Tumors
Chest pain or discomfort
- May present as dull or sharp pain, often caused by the tumor pressing on surrounding structures.
Enlarged lymph nodes
- Tumors may grow large enough to be palpable or visible on imaging studies.
Arrhythmia
- Irregular heartbeat may occur if the tumor affects the heart or its electrical conduction system.
Endocrine-related symptoms
- Myasthenia gravis – An autoimmune disorder where antibodies block or destroy acetylcholine receptors, leading to muscle weakness.
Symptoms of mediastinal compression
- Superior vena cava syndrome – Tumor compression of the superior vena cava may cause venous congestion in the head, neck, and upper limbs, leading to swelling and distended veins.
Neurological symptoms
- Hoarseness – May occur if the tumor compresses the recurrent laryngeal nerve, causing vocal cord paralysis.
- Dysphagia (difficulty swallowing) – May result from esophageal compression.
Systemic symptoms
- Fever – May be due to tumor-related infection or inflammation.
- Unexplained weight loss – Common in larger or malignant tumors.
- Fatigue – Persistent tiredness that is not relieved by rest.
Respiratory symptoms
- Cough – Often dry and persistent.
- Shortness of breath (dyspnea) – Especially if the tumor compresses the trachea.
- Stridor – A high-pitched sound during breathing, usually due to airway obstruction.
- Hemoptysis (coughing up blood) – Rare, but possible if the tumor invades blood vessels.
Imaging Tools for Diagnosing Mediastinal Tumors
- Chest X-ray: Useful for initial screening, but may miss tumors in the anterior or posterior mediastinum due to overlapping shadows from the heart and spine.
- Computed Tomography (CT scan): Clearly reveals tumor size, location, and involvement of vital organs or blood vessels. It is the primary imaging tool for preoperative planning.
- Magnetic Resonance Imaging (MRI): Especially helpful for evaluating nerve sheath tumors arising near the spinal cord or sympathetic chain. MRI helps determine whether the tumor extends through the neural foramina into the spinal canal.
Types of Mediastinal Tumors
Benign Tumors
- Lipoma
- Intrathoracic Goiter
- Cysts – Including bronchogenic cysts and pericardial cysts.
- Mature Teratoma – Well-differentiated tumors containing tissues like hair, skin, and fat.
- Benign Neurogenic Tumor – Tumors arising from peripheral nerves such as spinal, intercostal, or sympathetic nerves.
Malignant Tumors
- Immature Teratoma – Poorly differentiated and more likely to be malignant.
- Metastatic Tumors – Cancers from other parts of the body (e.g., lung or breast) that spread to the mediastinum.
- Primary Malignant Tumors – Includes thymoma, thymic carcinoma, lymphoma, and malignant neurogenic tumors.
Possible Causes of Mediastinal Lymphadenopathy
- Lymphoma
- Tuberculosis – Caused by Mycobacterium tuberculosis, commonly affecting mediastinal lymph nodes.
- Sarcoidosis – An inflammatory condition that forms granulomas, especially in the lungs and mediastinal nodes.
- Metastatic Cancer – Malignancies from other organs that spread to mediastinal lymph nodes.
- Esophageal Cancer – Tumors involving the mediastinal portion of the esophagus.
- Achalasia – A disorder where the lower esophageal sphincter fails to relax, causing esophageal dilation within the mediastinum.
- Esophageal Diverticulum – A pouch-like outpouching of the esophageal wall that can vary in size and location.
- Pneumo-Mediastinum – Air in the mediastinum due to trauma (e.g., rib fractures, tracheal injury) or spontaneous lung rupture.
- Aortic Aneurysm – Abnormal dilation of the aorta within the mediastinum, often caused by hypertension, atherosclerosis, or connective tissue disorders.
- Aortic Dissection – A life-threatening tear in the aortic wall causing sudden, severe chest pain.
- Superior Vena Cava Syndrome (SVCS) – Obstruction or narrowing of the superior vena cava, usually from tumors or thrombosis, leading to swelling of the face, neck, and upper limbs.
- Congenital Diaphragmatic Hernia – A birth defect where abdominal organs herniate through the diaphragm into the mediastinum.
- Myasthenia Gravis – A chronic autoimmune disease where antibodies disrupt acetylcholine receptors, leading to muscle weakness and fatigue.
- Systemic Lupus Erythematosus (SLE) – Can cause inflammation in vessels, heart, or lungs that may affect the mediastinum.
- Rheumatoid Arthritis – An autoimmune disorder that may lead to inflammation in tissues and joints, potentially extending to the mediastinum.
Get Expert Care forMediastinal Tumors
Surgical Treatment Options for Mediastinal Tumors
The choice of surgical approach for mediastinal tumors depends on the tumor's size, location, and extent of invasion into surrounding structures.
If the tumor is malignant, further treatment—such as chemotherapy or radiation therapy—may be required based on tumor staging.
Surgical resection is considered only when the tumor does not invade critical nearby organs or vessels. Available surgical methods include:
- Median sternotomy or traditional open thoracotomy
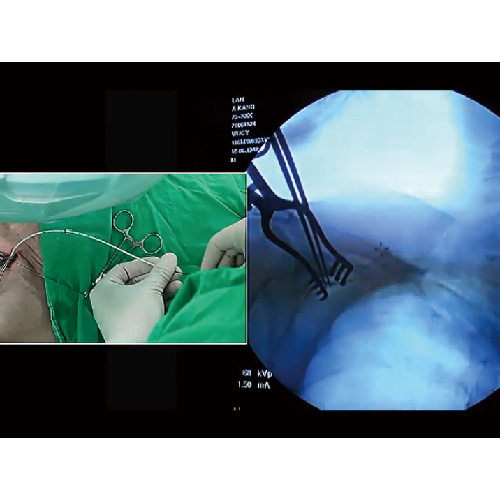
- Uniportal or multiport video-assisted thoracoscopic surgery (VATS)
- Robotic-assisted thoracic surgery
Since each patient's condition is unique, the choice of surgical technique should be discussed in detail with a thoracic surgeon.
Mediastinal Tumor Surgery Process
-
 1
1Cardiopulmonary Evaluation
-
 2
2Disease Severity Evaluation
-
 3
3Surgical Planning and Simulation
-
 4
4Assess Extent of Invasion
-
 5
5Surgical Tumor Resection

Mediastinal Tumors FAQ
Is a Mediastinal Tumor Always Cancer?
Not all mediastinal tumors are cancerous (i.e., malignant). Some are benign and pose minimal risk, while others are malignant and may require aggressive treatment. Here are examples of malignant mediastinal tumors that are considered cancer:
‧ Primary Malignant Tumors
‧ Thymoma
‧ Thymic Carcinoma
‧ Lymphoma
‧ Malignant Neurogenic Tumor
‧ Immature Teratoma
‧ Metastatsic Carcinoma
How Much Does Mediastinal Tumor Surgery Cost?
The cost of mediastinal tumor surgery generally includes two main components:
‧ Surgical fees – These are mostly covered by national health insurance, with the patient responsible only for a partial out-of-pocket co-payment.
‧ Self-pay surgical materials – Costs vary depending on the surgical technique used, such as median sternotomy, traditional open surgery, uniportal or multiport VATS, or robot-assisted surgery. Each approach requires different instruments and materials, which can affect the overall cost.
It is recommended to consult your thoracic surgeon before surgery to receive a detailed explanation of your treatment plan and an accurate cost estimate.
Does a 10 cm Mediastinal Tumor Require Surgery?
Tumor size often influences the size of the surgical incision needed. A 10 cm mediastinal tumor typically requires a larger incision to allow for safe removal.
Large mediastinal tumors also raise concerns about malignancy and may compress vital structures such as the trachea or blood vessels, leading to clinical symptoms. In such cases, surgical removal is usually indicated.
Because the mediastinum is located near major blood vessels, biopsy of these tumors can be challenging and risky. If imaging shows no invasion into critical structures, surgical resection is often recommended—both to remove the tumor and to obtain a definitive tissue diagnosis.
Is the Survival Rate for Mediastinal Tumors High?
The survival rate for mediastinal tumors largely depends on whether the tumor is benign or malignant.
Benign tumors generally have an excellent prognosis and can often be completely removed through surgery. In the case of malignant tumors, prognosis varies based on whether the tumor is primary or metastatic, and several additional factors influence survival:
Primary Malignant Tumors
‧ Tumor stage – including local invasion and distant metastasis
‧ Response to treatment – tumors that respond well to surgery, chemotherapy, or radiation tend to have better outcomes
‧ Age and overall health – patients in good health are usually more tolerant of aggressive therapies, which improves prognosis
Metastatic Tumors
‧ Oligometastases – If metastases are limited and visible on imaging, local control (e.g., tumor ablation, surgery, or radiation therapy) combined with systemic therapy (chemotherapy, immunotherapy, or targeted therapy) may significantly improve survival, even in advanced-stage disease.
‧ Disseminated metastases – When metastases are widespread, treatment typically involves only systemic therapy. Prognosis then depends on how well the tumor responds to chemotherapy, immunotherapy, or targeted drugs.
PressCoverage
 Health LTN
Health LTN
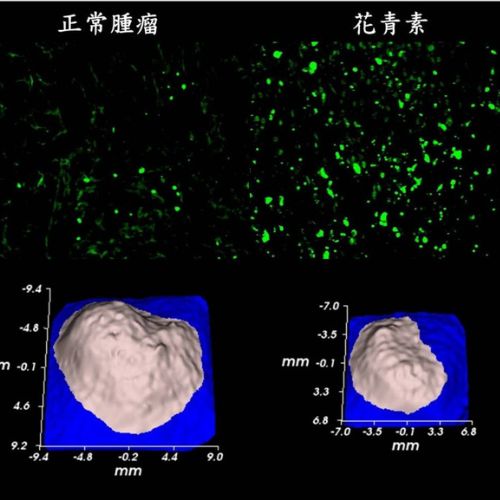
Advancing Large-Cell Lung Cancer Treatment: NCYU & Chang Gung Memorial Hospital, Linkou Collaborate
Associate Professor of NCYU and Dr. Wu’s team collaborate on large-cell lung cancer research, yielding significant findings...
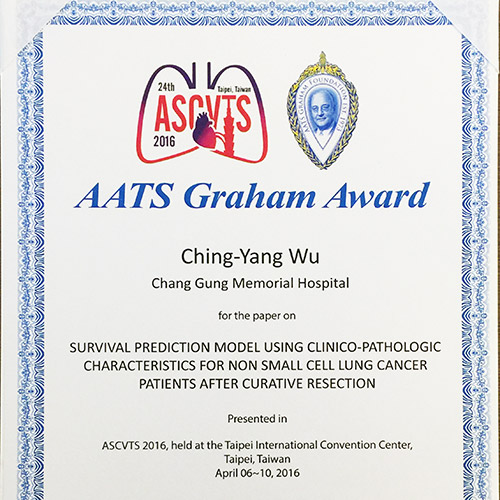
Dr. Wu Receives AATS Graham Award at ASCVTS 2016
Dr. Wu excelled in the AATS Graham Award evaluation, delivering his research within the 12-minute limit (10-minute presentation + 2-minute Q&A)...
Dr. Wu’s Team Publishes Study on Three CT-Guided Techniques for Lung Lesion Localization in the European Journal of Radiology!
From September 2019 to August 2021, the team analyzed 418 patients with lung lesions, comparing three CT-guided...
Dr. Wu’s Team Publishes Study on 3D Simulation Training for Oncology Nurses in Seminars in Oncology Nursing!
Since implantable venous catheters are not visible to the naked eye and can only be identified by touch, improper handling may occur...
Dr. Wu’s Research on Implantable Venous Ports Published in Medicine!
Based on literature and clinical experience, Dr. Wu formulated a standard algorithm to evaluate the best entry vessel for...
Dr. Wu’s Lung Cancer Research Published in Medicine!
Many patients still experience recurrent non-small cell lung cancer (NSCLC). To investigate, Dr. Wu and his team reviewed data from 356 stage I lung cancer patients (2005–2011), finding...
Dr. Wu’s Team Publishes Prognostic Study on Lung Adenocarcinomas ≤2cm in the Journal of the Formosan Medical Association!
The study aims to identify unique prognostic factors with clinical significance. Retrospective analysis of cases from...

Dr. Wu’s Team Publishes Study on Postoperative Circulating Tumor Cells as a Predictor of Lung Cancer Recurrence in Diagnostics!
With extensive experience in lung cancer surgery, Dr. Wu’s team investigated whether changes in circulating tumor cells (CTC)...
Dr. Wu’s Study on Central Venous Catheter Tip Placement Published in Medicine!
After analyzing 346 cases, Dr. Wu found that 221 cases (63.9%) were in the non-migration group, 67 cases (19.4%)...
Dr. Wu’s Research on a New Implantable Injection Port Published in Journal of Biomedical Materials Research Part B: Applied Biomaterials!
With in-depth studies and extensive clinical experience in implantable intravenous ports, Dr. Wu has explored complications...
Dr. Wu’s Expertise
- 2011 Taiwan Thoracic & Cardiovascular Surgery New Scholar Award
- 2012 Taiwan Thoracic & Cardiovascular Surgery President’s Award
- 2014 Taiwan Vascular Surgery Smart Award
- 2015 Taiwan Vascular Surgery Smart Award
- 2016 AATS Graham Award
- 2020 Taiwan Thoracic & Critical Care Medicine Best Paper
- 2021 Taiwan Thoracic & Cardiovascular Surgery President’s Award
- 2023 Global Injection Port Consensus Conference
InfoVideo
What Is a Port-A?
Port-A types can be classified by catheter material, high-pressure compatibility, and injection port material. Catheters are mainly made of silicone…

Why Get a Port-A?
A brief overview of the reasons for Port-A placement…

What Is a High-Pressure Port-A?
An overview of high-pressure Port-A and its clinical benefits…

How Do Healthcare Providers Use a High-Pressure Port-A?
Identification and injection procedure for high-pressure Port-A…

Post-Op Care for Port-A
Daily activities remain unrestricted, but certain movements depend on port placement…

Port-A Placement: What to Expect
An implantable venous port, commonly known as a Port-A, serves as a reliable IV access for clinical treatments. It functions like an invisible socket placed under the skin, allowing injection needles—like…